Chronic constipation is incredibly common. Around one in 4 people worldwide report symptoms, while in Australia and New Zealand, it’s around one in seven.
Lots of things can trigger constipation: being out of your usual routine (think holidays, illness or injury), having a low fibre intake, not drinking enough water and inactivity.
Certain medications may also cause constipation including iron supplements, painkillers, diuretics (to show you how to do away with sodium and water), and other drugs to treat heart disease, mental health conditions and allergies.
Constipation is more common in older adults and in womenattributable to hormonal changes that slow bowel motility – the time it takes in your body to digest food and expel the waste products (stools or bowel motions). Pregnant women are particularly vulnerable to constipation.
How do you’re constipated?
Symptoms include:
- lumpy or hard stools
- feeling that your bowels haven’t emptied completely or your anus is blocked
- straining to pass a bowel motion
- manipulating your body position to try to pass a bowel motion
- having fewer than three bowel motions per week.
If over a three-month period you answer yes to two or more of those symptoms most weeks, then you could have “constipation”.
The excellent news is it might be treated after which prevented.
Kongsak/Shutterstock
If your bowels are so packed you’ll be able to’t pass any bowel motions in any respect, see your GP. You may have treatment with specific laxatives to clear your bowels before you’ll be able to start on a prevention plan.
Here are 4 things that research shows improve bowel function, which refers back to the time it takes for food to maneuver through your digestive system and be expelled as a bowel motion (called gut transit time), the frequency and volume of bowel motions, and stool consistency.
1. High-fibre foods
Dietary fibres are complex carbohydrates that aren’t digested or absorbed within the gut.
Different varieties of dietary fibres improve bowel function through the next processes:
-
the fermentation of fibre within the colon produces water and other molecules. These make stools softer and easier to pass
-
absorption of water into stools stimulates the gut to contract and makes bowel motions softer
-
the next fibre intake creates larger stools, which pass more quickly, leading to more regular bowel motions.
A superb source of fibre is psyllium. It forms a viscous gel, which gets fermented within the colon, resulting in softer bowel motions. Psyllium is the foremost ingredient in Metamucil, which is often used to treat constipation.

Shawn Hempel/Shutterstock
A review comparing the effect of psyllium to wheat bran in individuals with chronic constipation found psyllium was 3.4 times simpler at increasing the quantity of stool passed.
This is vital because having an even bigger bowel motion waiting within the colon to be passed sends signals to your gut that it’s time to expel the stool – and it helps the gut contract to just do that.
The review found each psyllium and coarse wheat bran had a stool-softening effectbut finely ground wheat bran had a stool-hardening effect.
Other foods wealthy in fermentable carbohydrates include dark rye bread and legumes (chickpeas, lentils, four-bean mix, red kidney beans, baked beans); while wholemeal and wholegrain breads and cereals are high in various kinds of dietary fibres.
2. Kiwi fruit
Kiwi fruit fibre absorbs about thrice its weight in water. This means it helps make stools softer and boosts volume by increasing the quantity of water retained in bowel motions. This stimulates the gut to contract and moves the bowel motions along the gut to the anus.
In a study of 38 healthy older adultsresearchers found adding two to 3 kiwi fruit per day to their diets for 3 weeks resulted in participants passing bowel motions more often. It also increased the scale of their stools and made them softer and easier to pass.

Nitr/Shutterstock
Kiwi fruit are also wealthy within the complex carbohydrate inulin a variety of fructan. Fructans are a fibre, meaning they encourage growth of healthy bacteria within the colon.
But fructans may also aggravate symptoms in some individuals with irritable bowel syndrome (IBS). If you could have IBS and constipation, check in along with your GP before upping your fructan intake.
If you don’t like kiwi fruit, other vegetables and fruit high in fructans include spring onion, artichoke, shallots, leek, onion (brown, white and Spanish), beetroot, Brussels sprouts, white peaches, watermelon, honeydew melon and nectarines.
3. Prunes
Prunes are dried plums. They contain a considerable amount of sorbitol, a fancy carbohydrate that passes undigested into the colon where bacteria ferment it. This produces gas and water, which triggers a rise in bowel movements.
Eating prunes is even simpler than psyllium in improving stool frequency and consistency.
One study of adults with constipation compared eating 100 grams (about ten) prunes a day for 3 weeks to those that ate psyllium. The prune group passed a median of three.5 separate bowel motions per week in comparison with 2.8 within the psyllium group.
The prune group’s stools were also softer. They rated, on average, 3.2 on the Bristol stool chart in comparison with 2.8 for the psyllium group, meaning their bowel motions were more toward smooth to cracked sausage-shaped motions somewhat than lumpy ones.
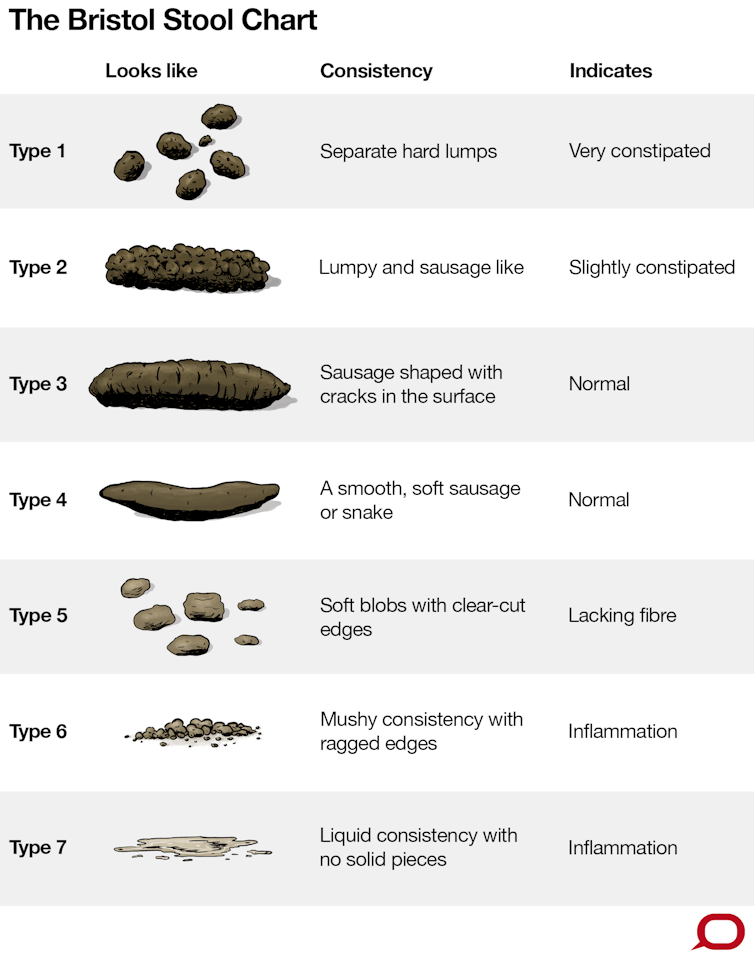
The Conversation, CC BY-ND
If you don’t like prunes, other foods that contain sorbitol include apples, pears, cherries, apricots, plums and “sugar-free” chewing gum and “sugar-free” lollies.
4. Water
Not drinking enough water is the strongest predictor of constipation. When your body is a bit dehydrated, there’s less water for the fibre in your colon to soak up, meaning your bowel motions also develop into dehydrated and harder to pass.
Aim for around 1.5 to 2 litres of fluid per day, which might include liquids similar to tea, coffee, soup, juice, and even jelly and the liquid from stewed fruit.
Putting all of it together
Start by increasing the quantity of water or other liquids you drink. You needs to be drinking enough that your urine is the color of straw.

Pixel-Shot/Shutterstock
Next, add in psyllium. Start with a tablespoon once a day with breakfast cereal.
Psyllium forms a gel as soon because it comes into contact with liquids so to make psyllium more palatable, mix it with a small amount of stewed fruit or yoghurt and eat it immediately. If needed, increase psyllium to twice a day.
At least once a day, have some prunes (either dried or canned) or kiwi fruit and quite a lot of other foods high in fibre, fructans, sorbitol and fermentable carbohydrate.
If your bowel habits don’t improve, see your GP.





