Possibly the earliest account of a disturbed mind is recorded in a 3,500-year-old Hindu text that describes a person who’s “gluttonous, filthy, walks naked, has lost his memory and moves about in an uneasy manner”.
In the Bible’s Old Testament, in the primary Book of Samuel, we read that King David simulated madness to realize safety:
And he modified his behaviour … and feigned himself mad of their hands, and scrabbled on the doors of the gate, and let his spittle fall down upon his beard.
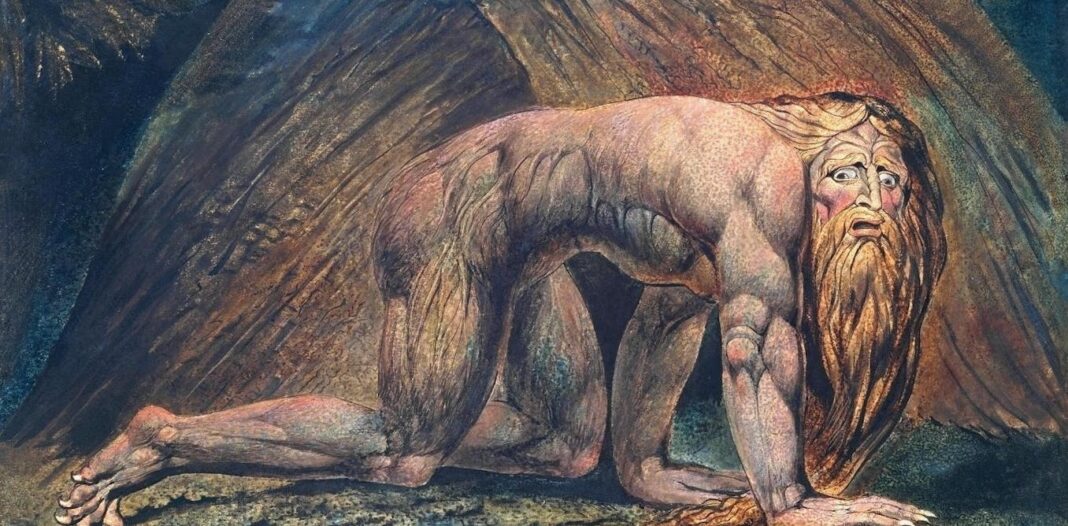
In the Book of Daniel, we discover a vivid description of King Nebuchadnezzar’s mental state:
And he was driven from men, and did eat grass as oxen, and his body was wet with the dew of heaven, till his hairs were grown like eagles’ feathers, and his nails like birds’ claws.
The ancient Greeks made early attempts to clarify madness. In the fifth century BC, Hippocrates viewed it as seated within the brain and influenced by 4 bodily fluids: blood, phlegm, black bile and yellow bile.
The Greek physician Galen, who practised in Rome 600 years later, argued that depression was brought on by an excess of black bile (hence the term “melancholia”, from , black, and , bile).
His contemporary, Aretaeus of Cappadocia, colourfully described how, if black bile moves upwards within the body, “it forms melancholy; for it produces flatulence and eructations [or, belches] of a fetid and fishy nature, and it sends rumbling wind downwards, and disturbs the understanding”.
A troubled mind, possessed
During the Middle Ages, monasteries preserved the view of madness as an illness, and of those afflicted as sick reasonably than sinful. At the identical time, the more sinister belief that the principal cause of the troubled mind was possession by spirits or the devil prevailed.
Sufferers were taken to sanctioned healers for exorcisms, a practice still carried out today in some cultures. People who failed to answer such treatment might then search out a celebrated expert.
Consider Hwaetred, a young man living in what’s now England within the seventh century, who became tormented by an “evil spirit”. So terrible was his madness that he attacked others together with his teeth and killed three men with an axe after they tried to restrain him. Taken to several sacred shrines, he obtained no relief. His despairing parents then heard of Guthlac, a monk who lived a hermit life north of Cambridge. After three days of prayer and fasting, Hwaetred was purportedly cured.
Wikimedia Commons
Over time, the role of spiritual authorities in mental illness dwindled, and the medical occupation claimed the exclusive practice of the healing arts. Insanity over again got here to be seen more as a physical malady than a spiritual taint. Even so, life for the mentally unwell could possibly be appalling.
During the seventeenth century, religiously inspired persecution of the mentally unwell was justified by the clerical hierarchy, and treatment was often some combination of neglect and bestial restraint.
Psychiatrists Martin Roth and Jerome Kroll describe the insane in this era as “miserable individuals, wandering around in village and in forest, taken from shrine to shrine, sometimes tied up after they became too violent”.
A watershed: asylums
The late 18th century was a watershed within the history of psychiatry. The insanity of England’s King George III revealed society’s ambivalence to the mentally unwell (vividly captured within the 1994 film The Madness of King George).
In France, Philippe Pinel released the chains that had fettered the “lunatic” for hundreds of years, ushering in an unprecedented phase of benevolent institutional care.
Moral therapy, a type of individualised care in small hospital settings, was promoted by English Quakers on the York Retreat and progressively supplanted inhumane physical treatments resembling purging, bleeding and dunking in cold water.
As populations grew and urbanised, the sheer numbers of mentally unwell people in burgeoning city slums demanded motion. An institutional solution emerged.
Asylums (from the Greek word meaning “refuge”) were in-built rural settings with the very best of intentions, planned to be havens by which patients would receive humane care. In the serenity of the countryside, and thru carrying out undemanding tasks, they could possibly be distracted from their internal torment and find dignity removed from the bustling crowd.
Daniel Defoe, the English author, remained unconvinced: “This is the peak of barbarity and injustice in a Christian country; it’s a clandestine Inquisition, nay worse.”
Although conceived in a spirit of optimism, asylums tended to deteriorate into centres of hopelessness and demoralisation. They soon became overcrowded dumps. Institutions built for just a few hundred people were soon holding hundreds. Very few residents were discharged; many stayed for many years. Brutal oppression replaced anything that may need resembled treatment; malnutrition and infectious disease became rife.
In the grim environment, people were shut away and forgotten. With them out of sight and out of mind, a lack of public interest and political neglect became the norm.

Wellcome Collection
The brooding constructing on the hill got here to symbolise the stigma and fear attached to mental illness. By the mid-Nineteenth century, critics were voicing concerns that asylums had turn into human warehouses that entrenched mental illness reasonably than curing it.
The combination of powerless patients, hospitals run more for the convenience of staff than for the good thing about the sick, inadequate inspection by state bodies, and lack of resources led at times to quite disgraceful conditions. Unwittingly, the spread of asylums also triggered the movement of psychiatry away from the mainstream of drugs.
The conditions of the asylums are evocatively described in Henry Handel Richardson’s Australian novel The Fortunes of Richard Mahony. We read of Richard’s decline, probably from syphilis affecting the brain, which at the moment afflicted a big proportion of mental patients.
Towards the tip of the novel, his wife comes to go to him within the asylum:
She hung her head … while the warder told the story of Richard’s misdeeds. 97B was, he declared, not only disobedient and disorderly, he was extremely abusive, dirty in his habits … he refused to scrub himself, or to eat his food … she had to maintain a grip on her mind to hinder it from following the image up: Richard, forced by this burly brute to grope on the ground for his spilt food, to scrape it together, and either eat it or have it thrust down his throat … There was not only feeding by force, the straitjacket, the padded cell. There were drugs and injections, given to maintain a patient quiet and ensure his warders their freedom.
Great and desperate cures
In the asylum, psychiatry become a contemporary medical discipline. The
accumulation of hundreds of patients provided the primary opportunity
to review mental illness systematically and to develop theories about its
causes.
The concept that these conditions were attributable to brain alterations, and particularly degenerative processes, became dominant, encouraged by the invention of the cerebral pathology related to neurosyphilis and Alzheimer’s disease. An analogous degenerative process was proposed by the good German psychiatrist Emil Kraepelin to cause dementia praecox – later renamed “schizophrenia” – resulting in pessimism about the potential for recovery.
But the priority for asylums was to alleviate the suffering of overwhelming numbers of disturbed patients. Psychiatrists grasped for “great and desperate cures”. Henry Rollin, an English psychiatrist and medical historian, captures the extraordinary zeal:
The physical treatment of the frankly psychotic during these centuries makes spine-chilling reading. Evacuation by vomiting, purgatives, sweating, blisters, and bleeding were considered essential […] There was indeed no insult to the human body, no trauma, no indignity which was not at one time or other piously prescribed for the unlucky victim.
Treatments were sometimes based on rational grounds. Malaria therapy, as an example, was launched as a treatment for neurosyphilis by the Viennese psychiatrist Julius Wagner-Jauregg in 1917, earning him a Nobel Prize ten years later.
The high fever brought on by the malarial parasite disabled the spirochete that caused neurosyphilis, however the hope that it might be equally effective for other types of psychosis was soon dashed. The wished-for panacea was to not be.

Jimmy Chan/Pexels
Insulin-coma therapy was introduced by Manfred Sakel within the Thirties in Vienna and was soon getting used in lots of countries to treat schizophrenia. An insulin injection was administered six days every week for several weeks, producing a state of sunshine coma lasting about an hour, due to reduced glucose reaching the brain.
Many years later, an investigation carried out within the Institute of Psychiatry in London, a number one research centre on the time, showed conclusively that the coma itself was of no therapeutic value. Any positive change was probably attributable to the staff’s painstaking care.
ECT and lithium
The first widely available and effective biological treatments for mental illness were developed within the asylum. The discovery in 1938 of electroconvulsive therapy (ECT) by Ugo Cerletti and Lucio Bini, two Italian psychiatrists, led to a dramatically effective treatment for individuals with severe depression.
ECT was eagerly adopted in practice, but its history illustrates a typical pattern of treatment in psychiatry: unbridled early enthusiasm is later tempered by a protracted strategy of scientific evaluation.
The same will be said of using brain surgery to change psychiatric symptoms. This was pioneered in 1936 by Portuguese neurologist António Egas Moniz (one other Nobel Prize winner in the sector of psychiatry) and surgeon Almeida Lima, and stays controversial in psychiatry to at the present time.

Kurt Hutton/Picture Post/Hulton Archive/Getty Images
A momentous breakthrough was the invention in 1949 by John Cade, an Australian psychiatrist, of lithium as a treatment for manic excitement. The lithium story reveals how the incorporation of a brand new medication into psychiatric practice will not be at all times smooth.
Several US and Danish psychiatrists had experimented with lithium within the 1870s and Eighteen Nineties, only to have their work ignored until Cade’s rediscovery. It was one other 18 years before lithium was shown to stop the reoccurrence of severe changes of mood, its primary clinical use now.
Major tranquillisers were added to the growing range of psychiatric medications after being discovered fortuitously in 1953. An antihistamine used to calm patients undergoing surgery was shown to scale back the torment of psychotic patients, but without making them sleepy.
Shortly after this, the US psychiatrist Nathan Kline discovered that a drug being tested for its effect in patients with tuberculosis had antidepressant properties — the forerunner of medicines for depression. All these drugs radically transformed the practice of psychiatry.
Freud, ‘talking cures’ and shell shock
A really different aspect of mental health care arose within the Eighteen Nineties, outside
the asylum. Concerned with neurotic conditions, the brand new treatment grew chiefly out of neurology but was also influenced by a scientific interest in hypnosis and the unconscious.

Max Halberstadt/Wikimedia Commons
Sigmund Freud conceived a dynamic model of the mind by which, through the mechanism of repression, painful or threatening emotions, memories and impulses are prevented from escaping into conscious awareness.
Psychoanalysis grew to turn into an integrated set of concepts about normal and abnormal mental functioning and personality development, and spawned a brand new approach to psychologically based treatment. Psychoanalysis emerged as a serious theoretical underpinning of latest “talking cures” (psychotherapies), and its influence spread far beyond treating mental ill-health.
Both world wars profoundly influenced the sector. The high incidence of “shell shock” in World War I drove home the lesson that mental illness could affect not only those genetically predisposed, but even the supposedly robust. It soon emerged that anyone exposed to traumatic experiences was vulnerable.
A positive end result from World War II was the event of techniques for screening large numbers of recruits, which revealed the substantial prevalence of emotional problems amongst young adults.
The must treat quite a few psychiatric casualties led to the event of group therapies. These paved the way in which for the so-called therapeutic community, based on the concept that a complete ward of patients could possibly be an integral a part of treatment.
The idea of deinstitutionalisation began to assemble pace within the Nineteen Sixties, driven by a burgeoning civil-rights movement. Asylums, an influential book on the time by sociologist Erving Goffman, containing his minute observations of the sense of oppression experienced by patients in these “total institutions”, was one catalyst for his or her closure.
Hundreds of hundreds of long-stay patients began to be transferred to alternative accommodation and specialist care in the neighborhood, a process that remains to be in progress.
What is mental illness?
It is difficult to define what makes a pattern of behaviour and experience a mental disorder. Generally, such a pattern – or “syndrome” – is taken into account to be a disorder whether it is related to psychological distress, resembling intense and prolonged anxiety or sadness, or significant dysfunction, resembling a serious impairment in functioning in a number of key areas of each day life.
If the pattern is short-lived, relatively mild, or entirely comprehensible in light of the trials and tribulations of the person’s life, it must be seen as an issue in living reasonably than a mental disorder. Such problems should profit from consultation with a mental health skilled despite not being diagnosable disorders.
This definition of what counts as a mental disorder also clarifies what will not be a mental disorder. Merely being unusual or violating social norms doesn’t mean an individual has a disorder.
It is difficult sometimes to make a decision whether a brand new sort of behaviour is a mental disorder. For instance, should excessive smartphone use or compulsive gambling be counted as diagnosable addictions?

Dave Hunt/AAP
Troubling cases
These decisions about what to incorporate under the umbrella of mental illness are fraught, and there have been some troubling historical cases when disturbing decisions were made or proposed.
In the 1850s, for instance, Samuel Cartwright, a physician from Alabama, proposed a brand new diagnosis called “drapetomania” to clarify why African-American slaves would want to flee their servitude.
He really useful slaves must be treated kindly and humanely to stop the disorder, but whipped if this treatment failed. A more patent abuse of the concept of mental illness can be hard to assume, and it must be noted that other physicians ridiculed Cartwright’s proposal on the time.
Two other controversial cases date to the last century. In the early Nineteen Seventies, one among us (Sidney) stumbled across disturbing media reports that many political and spiritual dissenters and human-rights activists within the Soviet Union were being labelled as mentally unwell and detained in mental hospitals indefinitely or until they renounced their “disturbed ideas”.

Boris Spremo/Toronto Star/Getty Images
For instance, General Pyotr Grigorenko criticised the privileges of the Soviet elite and publicly espoused the rights of the Crimean Tatar ethnic minority group. He was diagnosed with paranoid tendencies, one symptom being his “reformist ideas”, and forcibly committed to a psychiatric facility.
In effect, Soviet psychiatry’s definition of mental illness, and psychosis particularly, was so broad that political views concerning the desirability of social change were recast as delusions.
The second case comes from the US. Until 1973, homosexuality was defined as a sexual deviation and included within the set of recognised mental disorders. Under pressure from civil, women’s and gay rights activists, it was faraway from the diagnostic manual.
Noting such cases, every time the boundary of a mental illness is expanded to incorporate recent diagnoses or loosen old ones, some critics will worry we’re treating normal behaviour as a pathology and that we are going to harm people by labelling them. And every time the boundary contracts, others will worry that folks with psychological troubles are being excluded from clinical care.
Deciding what’s and isn’t a mental illness is difficult, but has marked consequences.