Although COVID-19 was first described as a disease of the lungs, as its relentless march has continued we’ve realised that it has a far wider reach within the human body. COVID-19 has been related to skin rashes, bleeding disorders and structural damage to the center and kidneys. It has also been implicated in disorders of each the brain and the mind.
Early studies prompted fears that healthcare services would collapse under a crushing wave of strokes, brain inflammation and muscular disorders. Moreover, reviews of previous coronavirus outbreaks warned that those recovering from COVID-19 may face an increased burden of psychiatric disorders like depression and PTSD.
But despite research on COVID-19 and the brain being produced at unprecedented scale and speed through the pandemic – with a whole bunch of latest articles appearing every week – it was hard initially to search out reliable data to substantiate or disprove these fears.
So, as a team of doctors, students and researchers from disciplines including psychiatry, psychology and neurology, we joined forces to analyse all of the available research on the results of COVID-19 on the brain. By doing so, we aimed to chop through numerous the speculation surrounding COVID-19’s neurological and psychiatric effects. Here’s what we found.
Different conditions, different frequencies
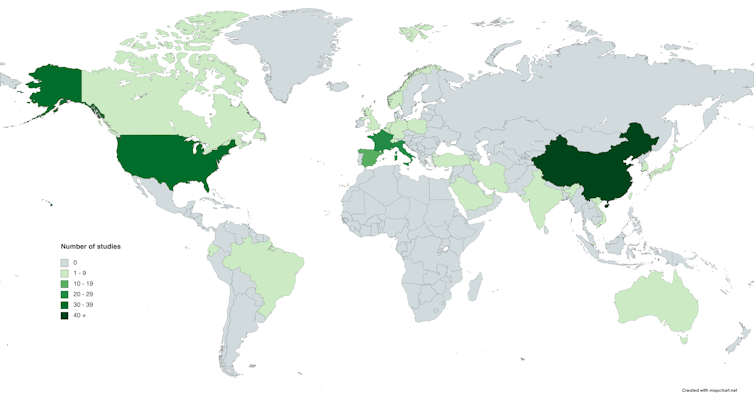
Our team soon realised that lots of the associations between COVID-19 and the brain were being drawn from small, highly chosen groups of patients, which risks bias. So to combat this, we whittled down the vast number of probably relevant papers on the neurology and psychiatry of COVID-19 (greater than 13,000) to 215 that were robust enough to be analysed. Collectively, these covered 105,000 people from 30 countries.
We found that in these studies essentially the most common neuropsychiatric symptoms were lack of smell (anosmia), weakness, fatigue and a change in taste (dysgeusia), which all occur quite ceaselessly. Anosmia and weakness appeared in greater than 30% of the patients the studies we checked out, for instance. It’s subsequently very likely that neuropsychiatric symptoms in COVID-19 are the rule and never the exception.
But reassuringly, initial fears about more serious brain-related conditions – reminiscent of widespread inflammation of the brain (encephalitis) and Guillain-Barré syndromewhere the immune system attacks the nerves – appeared to be based only on very rare events. Concerns about vast waves of such conditions seem unfounded.
aijiro/Shutterstock
However, we did find that some essential mental illnesses, reminiscent of depression and anxiety, were each occurring in as many as 25% of individuals with COVID-19. These may represent an enormous burden to patients in years to come back. Even neurological events reported less ceaselessly, like stroke (which occurred in about 2% of hospitalised patients), will still represent an unlimited challenge to patients and healthcare systems attributable to the sheer scale of this pandemic’s reach and the incontrovertible fact that they often have life-changing results.
Interestingly, we found that several symptoms (including muscle pain and lack of smell) were actually reported more commonly in those with less severe COVID-19 – the other of what you would possibly expect. Of course, there could also be a straightforward explanation for this: perhaps critically unwell patients are less prone to be probed about certain symptoms, particularly those which are less severe. We also saw many disabling symptoms (including fatigue and headache) present in those that weren’t hospitalised in any respect.
But answers are removed from final
While reading this, you will have been struck by a giant query surrounding all these studies: how can we know that COVID-19 is definitely causing any of those problems? Depression is common – might these people have developed it anyway without getting COVID-19? And what if having a psychiatric illness makes you more prone to get COVID-19? One large study with US data suggests that that is the case.
These are all real issues in the info available up so far, as unless you’ve a comparison group of people without COVID-19, it’s unimaginable to know whether the people you might be studying were going to have high rates of neuropsychiatric disorders no matter catching the coronavirus. Ideally, you wish a gaggle of individuals without mental illness as your baseline, and to then see what happens when a few of them are exposed to COVID-19.
Without such studies, it’s hard to attract any hard conclusions – and unfortunately almost the entire studies we checked out didn’t have comparison groups. However, we’re beginning to get some comparative data now. For example, we now know that individuals who’ve had COVID-19 are more likely than the overall population to develop a brand new mental illness. In addition, most psychiatric and neurological problems appear to be more common after COVID-19 than after flu.
Another issue is that the research done to date accommodates biases that may’t be eliminated. It’s biased towards patients in hospital, when most individuals with COVID-19 never go near a hospital. It’s biased towards acute illness, reasonably than the longer-term effects of COVID-19. And it’s biased towards China, the US and other western countries, with little known about what is going on in Africa or much of the Pacific region. To get a more comprehensive view, we’d like future research to have a wider scope.
Author provided
What we do know is that individuals with COVID-19 fairly often experience a variety of neurological and psychiatric problems, so healthcare providers need to organize not just for the immediate care of those patients, but in addition the intensive and sometimes lengthy rehabilitation needs that follow. Early research (yet to be reviewed by other scientists) is raising concerning signs of neuropsychiatric symptoms persisting many months following the onset of illness.
Finding out the true impact of COVID-19 on the brain is just a primary step. In reality, the disease’s neurological and psychiatric impacts are prone to pose a challenge to clinicians and healthcare systems for a few years to come back.





