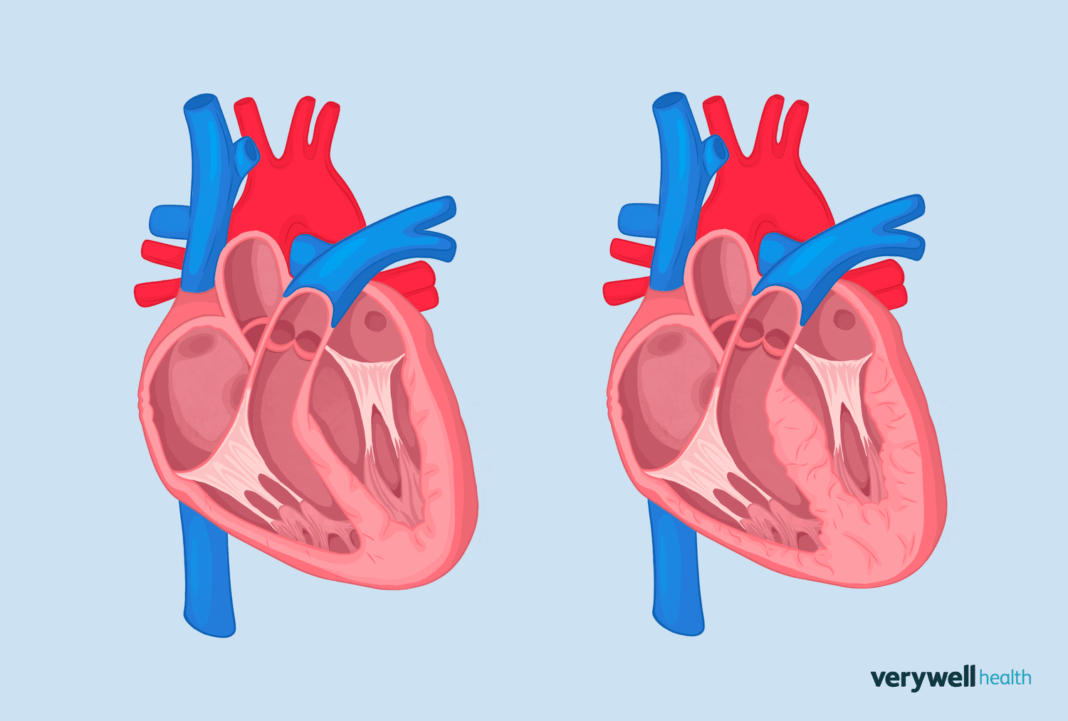
Left ventricular hypertrophy (LVH) is an increase in the mass (weight) of the left ventricle, which is the heart’s main pumping chamber. LVH develops either when the force or volume of blood within the ventricle becomes excessive. Common conditions that cause LVH are high blood pressure and aortic stenosis (a heart valve disease).
Since LVH often manifests silently over many years, it’s frequently diagnosed through a routine electrocardiogram (ECG). LVH can usually be reduced or reversed by treating the underlying cause, which entails adopting healthy lifestyle behaviors and taking medication or undergoing surgery.
Illustration by Zoe Hansen for Verywell Health
What Causes Anatomical Changes in LVH?
The left ventricle is one of the heart’s four chambers. It pumps oxygen-rich blood into the aorta, the largest artery in the body that delivers blood to vital organs.
Over time, the left ventricle undergoes natural remodeling, a process influenced by non-modifiable factors like normal aging and ethnicity and modifiable risk factors like high blood pressure (hypertension), diabetes, obesity, and metabolic syndrome (a group of conditions that occur together to increase risk of type 2 diabetes, stroke, and heart disease).
Left ventricular hypertrophy is a type of heart-related remodeling that involves an increase in the mass of the left ventricle.
LVH is a response to one or both of the following:
- Blood pressure overload within the LV causes an increase in wall thickness.
- Blood volume overload within the LV ventricle causes an increase in the chamber size.
Associated Conditions
Two of the most common causes of LVH are:
- Hypertension is when blood’s force, or impact, on artery walls is too high. Hypertension creates increased pressure within the left ventricle, causing the heart muscle to thicken as it works extra hard to pump blood into the aorta.
- Aortic stenosis narrows the aortic valve, interfering with blood flowing from the left ventricle into the aorta. The increased pressure within the left ventricle causes the walls to thicken.
Other causes of LVH include:
- Aortic regurgitation is when the aortic valve leaks, causing blood to reverse its flow (in the wrong direction) back into the left ventricle.
- Mitral regurgitation occurs when the mitral valve leaks, causing blood to reverse its flow (in the wrong direction) back into the left atrium (the upper chamber above the left ventricle).
- Dilated cardiomyopathy is characterized by stretching and enlargement of the ventricles (usually starting in the left and spreading to the right). Possible causes of this condition are coronary artery disease, alcohol, and infection.
- Hypertrophic cardiomyopathy is a condition that runs in families and is characterized by thickening of the walls of the left ventricle. This condition is the most common cause of sudden cardiac death in young individuals and competitive athletes in North America.
- A ventricular septal defect is a hole in the wall between the right and left ventricles. It’s the most common congenital (present at birth) heart disease. With a large VSD, blood wrongly flows from the left to the right ventricle, overwhelming the lung arteries and the left side of the heart. The left ventricle increases in size to compensate for the extra blood.
- An “athlete’s heart” refers to heart-related changes in athletes that manifest as an adaptation to intense physical training. Even though these heart-related changes can meet the criteria for left ventricular hypertrophy, they are considered harmless, as they differ pathologically from those caused by high blood pressure, for example.
Symptoms and Onset
Left ventricular hypertrophy usually causes no symptoms for many years.
Over time, as the left ventricle thickens and/or enlarges, the heart muscle becomes weaker and stiffer and is unable to pump blood very well.
Left-sided heart failure may then occur, causing the following symptoms:
How Serious Is LVH?
LVH is a concerning finding because it indicates that a person’s heart is working harder than usual. Depending on the severity of the LVH and its cause, the heart may not be pumping blood efficiently.
In addition to heart failure, LVH is associated with the following complications:
ECG Findings
An electrocardiogram (ECG or EKG), which assesses the heart’s electrical activity, is a readily available tool to detect LVH.
During an ECG, a person lies on a bed or table, and small, sticky pads are strategically positioned on the chest, arms, and legs. Wires attach the pads to a machine, translating the heart’s electrical activity onto paper. The paper is divided into large and small boxes to calculate time and distance.
The heart’s electrical activity appears like wavy, spiky lines on the paper.
These lines consist of the following three parts:
- The P wave represents blood being pumped from the atria (the heart’s upper chambers) into the ventricles (the heart’s lower chambers).
- The QRS complex consists of three waves and represents blood being pumped out of the heart (into the lungs or the aorta).
- The T wave represents the ventricles relaxing before the above “pumping blood” cycle repeats itself.
Many different criteria for ECG findings in LVH have been developed, although five general findings of LVH are:
- An elevation of the QRS voltage (height of the waves) occurs because there are more muscle fibers within the left ventricle for the electrical signals to travel through.
- The QRS complex widens because electrical signals travel a longer path within the left ventricle.
- Left axis deviation occurs because the direction of the electrical activity moving through the heart is distorted towards the left.
- ST changes occur when electrical signals move differently through the left ventricle due to its remodeling. This finding can mimic that seen with an ST-elevation (“STEMI”) heart attack (when an artery that feeds the heart muscle is completely blocked).
- Left atrial abnormality is seen with thickening, widening, or both of the left atrium, occurring as a response to chronic left ventricular hypertrophy.
Keep in mind that while an ECG is a reasonable “first-step” tool for identifying LVH and eventually monitoring LVH, imaging tests can more accurately diagnose the condition and its underlying cause.
These imaging tests include:
- An echocardiogram is an ultrasound of the heart muscle. It uses sound waves to visualize the heart’s size, shape, thickness, movement, pumping ability, and how well the valves are working.
- Cardiac magnetic resonance imaging (MRI) uses magnetic fields and radio waves to produce three-dimensional images of the heart. It offers a more precise evaluation of left ventricle structure and function than an echocardiogram.
Does Treatment Reverse LVH?
Depending on the cause, LVH can be reduced or reversed—a term called LVH regression. For example, if LVH is caused by high blood pressure, lowering the blood pressure can lead to LVH regression.
Even better, research suggests that LVH regression improves cardiovascular prognosis with intensive blood pressure lowering, specifically maintaining a blood pressure lower than 120/80 mm Hg (millimeters of mercury).
Classes of medications used to lower blood pressure include:
Similarly, if LVH is caused by a heart valve problem, like aortic stenosis, surgery to repair or replace the valve may be performed to achieve LVH regression and improve the heart’s functioning.
Bottom Line: LVH Regression Improves Prognosis
Achieving LVH regression through medication or surgery decreases the risk of severe complications like heart attack and stroke.
Importance of Lifestyle Changes and Habits
If you or a loved one has LVH, treatment is directed at managing or fixing the underlying cause. While medication and/or surgery may be indicated, adopting heart-healthy lifestyle behaviors also plays a key role.
Heart-healthy behaviors include:
- Maintaining a healthy weight
- Exercising (under the guidance of a healthcare provider if you have heart/lung/joint or other health problems)
- Eating heart-healthy foods like fruits and vegetables and limiting excess salt
- Avoiding smoking and limiting or avoiding alcohol
- Appropriately managing causes of underlying LVH causes (e.g., taking high blood pressure medication as instructed)
Summary
Left ventricular hypertrophy (LVH) is an increase in the weight of the left ventricle due to thickening of the left ventricle walls, an increase in space within the left ventricle, or both. The two most common causes of LVH are high blood pressure and aortic stenosis (a heart valve disease).
LVH symptoms are usually silent for years until the heart weakens and stops pumping blood efficiently. Once the left heart begins to fail, symptoms like trouble breathing, chest pain, fatigue, and dizziness develop.
LVH can be diagnosed with an electrocardiogram (ECG), echocardiogram (ultrasound of the heart), or a cardiac MRI (three-dimensional images of the heart), usually before symptoms even develop.
LVH can often be fixed by treating the underlying cause—for example, intensively lowering high blood pressure or repairing/replacing a faulty aortic valve. Engaging in heart-healthy habits like weight loss if overweight or having obesity and staying physically active are also essential to maintaining a structurally and functionally healthy left ventricle.
If underlying causes of LVH are not addressed, potentially life-threatening problems may develop, like heart attack, stroke, or abnormal heart rhythms.





Fantastic site A lot of helpful info here Im sending it to some buddies ans additionally sharing in delicious And naturally thanks on your sweat